A team including researchers at the IGTP confirm new ways to test and treat TB by harnessing the body’s own defences
In new study in a cohort of patients from Southern Europe, researchers including the innovation in Respiratory Infections and Tuberculosis Diagnosis Group at the IGTP have confirmed the importance of exploring immune pathways other than the ones modulated by interferon-gamma, which is the one that has been most studied in work on TB until now. The study published in Frontiers of Immunology has also hinted at ways to differentiate between latent and active TB, a major goal in the battle against the disease.
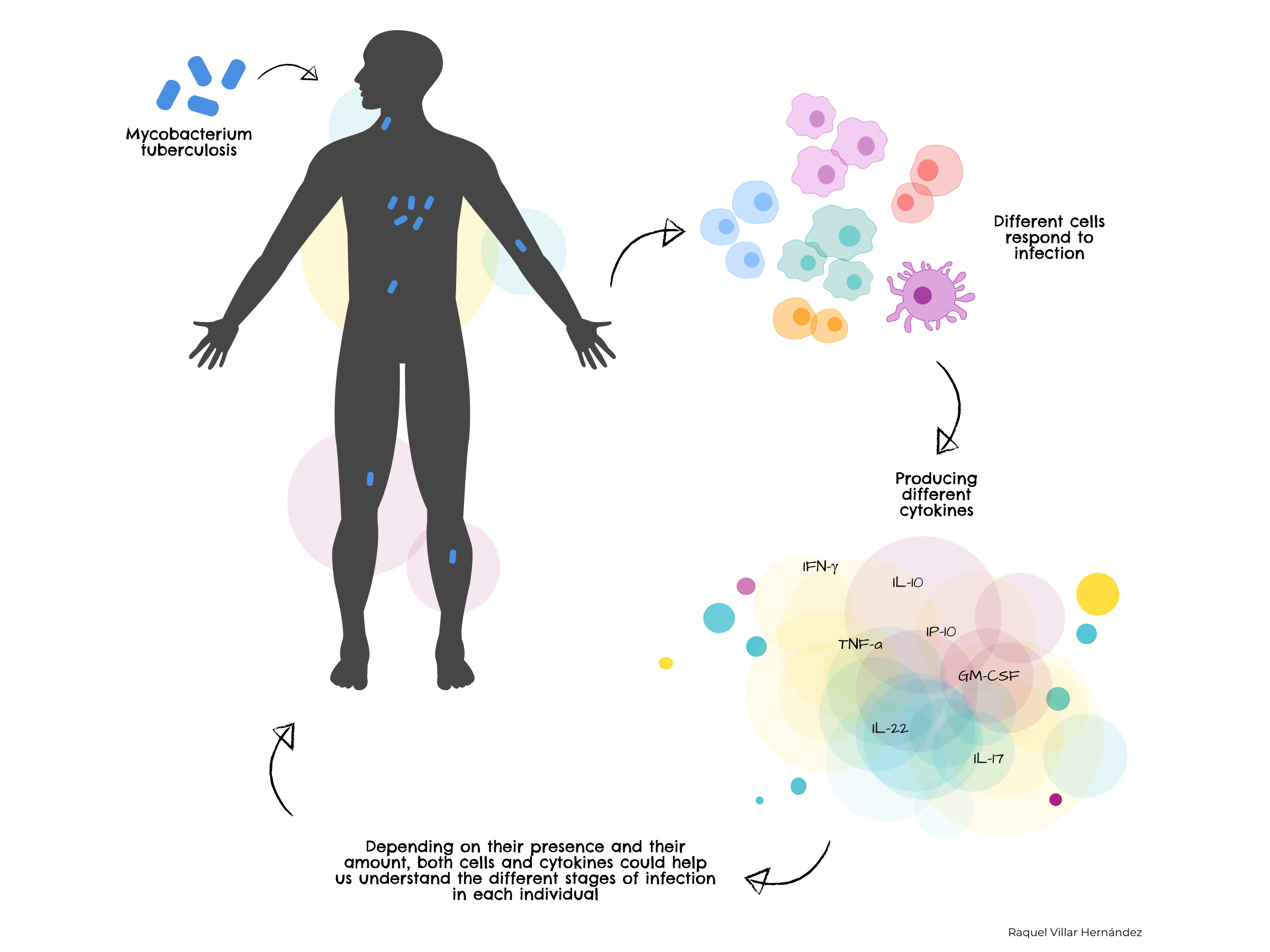
Tuberculosis, or TB, is caused by the bacteria Mycobacterium tuberculosis. An important part of the defence against TB focusses on cytokines, substances used by immune cells to communicate and control the immune response. Until now, a large amount of work concentrated on one cytokine, interferon-gamma. This research confirms that different cytokines previously identified by the group are also key in fighting TB in the patients in the study. What is more, they may be useful in discriminating between active and latent infections and predicting the progression of the disease.
"TB is a difficult disease to diagnose and treat and is more widespread than people imagine, a quarter of the world's population is estimated to be latently infected, which means that it is not active, or making them ill, but it can progress to active so it does make them ill and then they can pass it on to other people," explains José Dominguez, of the Innovation in Respiratory Infections and Tuberculosis Diagnosis Group at the IGTP, which worked with several European research groups, including the University of Leiden, the CIBER Network and many hospitals on this study. "Immunodiagnostic tests currently available don't discriminate between latent infections and those in which the bacteria is active in the lungs." An additional problem is that there is currently only one vaccine, which protects small children, but does not stop active TB in the lungs for adolescents and adults, so even after vaccination, they continue to spread the disease.
The immune system can be compared to a complex game of cat and mouse between invading microorganisms and the body's own defences. Part of the bacteria's strategy is to "hide" from the immune system in several ways. Substances called antigens located on the bacteria M. tuberculosis that cause tuberculosis (TB) are recognized by specialized cells in the immune system, which martials its defences using cytokines, amongst other substances. Until now, much research concentrated on the cytokine interferon-gamma, which is known to be involved in the body's defence.
The group had previously identified different antigens from M. tuberculosis in lung tissue samples and different cytokines produced by immune cells in response to them. Some of these cytokines and associated immune cell type are more common in adults with the disease and others in adolescents. Additionally, they could also be markers for active and latent TB.
“This is a small study, but with very relevant results,” says Raquel Villar-Hernández. “It confirms our results in the laboratory and shows that we must assess a wider range of immune responses to TB, not just interferon-gamma. Also, we should continue to investigate both cytokines and populations of different immune cells as a means of not just detecting TB, but stratifying patients of different ages into groups at different stages of the disease.”
Original paper
Mariateresa Coppola et al, Front Immunol. 2020; 11: 103. Published online 2020 Feb 11. doi: 10.3389/fimmu.2020.00103, PMCID: PMC7026259, PMID: 32117257
Funding
This study was supported by the European Commission [FP7 NEWTBVAC project contract no. LSHP-CT-2003-503367, EC ITN FP7 VACTRAIN project; EC HORIZON2020 TBVAC2020 (Grant Agreement No. 643381)]. It was also supported by: (i) a grant from the Instituto de Salud Carlos III (PI16/01912 and PI18/00411), integrated in the Plan Nacional de I+D+I and cofunded by the ISCIII Subdirección General de Evaluación and the Fondo Europeo de Desarrollo Regional (FEDER); and (ii) a grant from the Sociedad Española de Neumología y Cirugía Torácica (project 25/2016; SEPAR; Barcelona, Spain). AS-M was supported by a Juan Rodés (JR18/00022) postdoctoral fellowship from ISCIII. We acknowledge the support of the European Respiratory Society (Fellowship STRF 2016).
